Social and economic conditions such as housing, food security, employment, and education can account for as much as 80 percent of health outcomes and are increasingly being recognized as an important driver of health care costs.1
UPMC Health Plan seeks to serve our community and shape the health care system of tomorrow as part of UPMC's integrated delivery and finance system. Our goal is to provide members with the right care, in the right way, at the right time. Success with this goal often depends on many social factors, referred to as social determinants of health (SDOH).
In December 2019, the UPMC Center for Social Impact, in collaboration with the UPMC Center for High-Value Health Care, launched to coordinate, evaluate, and expand programming and innovations that address both the social needs and social determinants of the members and communities UPMC serves.
Recent news
New ideas for better health care

Good Health, Better World
Good Health, Better World Podcast
Freedom House Graduates
Freedom House 2.0 Graduates Set to Enter the Workforce as Health Care WorkersWhat are social determinants vs. social needs?
The national conversation around health care reform continues—and with it, an increased interest in wellness and prevention. SDOH, a concept that has been around for at least a decade, gained traction in the health care industry in 2019 as an upstream way to achieve more value-based care.
SDOH, as defined by the World Health Organization, are “the conditions in which people are born, grow, live, work, and age and are shaped by the distribution of money, power, and resources”.2 Social determinants tend to be systemic, societal challenges that will be solved through long-term upstream investments and collaboration between government, the public sector, and private industry.
A similar concept is social needs. In the context of health care, these are immediate barriers a member or patient faces in accessing the care they need. Many headline-grabbing health care investments to date that have been framed as addressing social determinants are instead meeting an immediate social need.
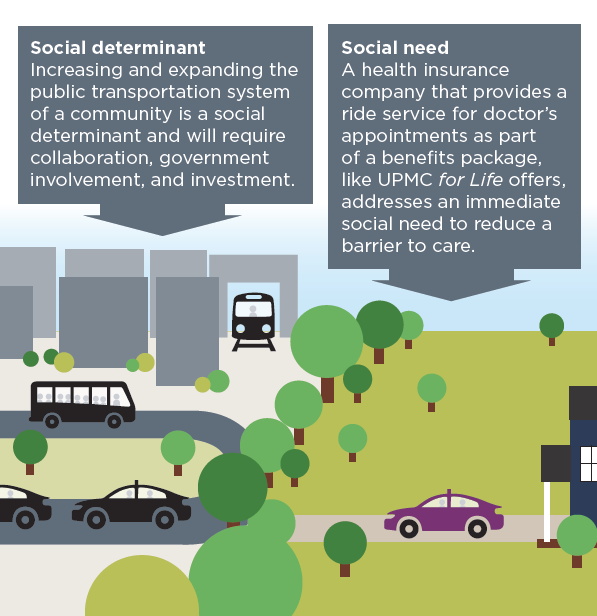
Increasing and expanding the public transportation system of a community is a social determinant and will require collaboration, government involvement, and investment. A health insurance company that provides a ride service for doctor’s appointments as part of a member’s health insurance benefits addresses an immediate social need to reduce a barrier to care.
What we’re working on
UPMC Health Plan is already leading the industry in transforming care delivery and the health care ecosystem through innovation, and our commitment to social initiatives goes back at least a decade. Social Impact focuses on three key domains: addressing social needs, coordinating and expanding access to benefits, and supporting underserved communities. Examples of initiatives in the communities UPMC serves include:
- Increasing employment and workforce development opportunities.
- Advancing affordable housing service coordination and rural health care.
- Supporting individuals with unique health needs, such as members of the LGBTQA+ communities.
At UPMC Health Plan, we believe that access to affordable, stable housing is crucial to long-term physical and mental health as well as an individual’s well-being. Evidence shows that stable housing positively impacts health outcomes and may also provide a critical foundation for addressing other social influencers on health, such as education, food security, and health care affordability and access.3,4,5,6
Our Cultivating Health for Success program connects our members in need of housing with the support they need while wrapping around services to enable access to physical and behavioral health care. To date, this program has served more than 100 members.
Through the Accelerating Investment in Health Communities initiative, UPMC Health Plan continues to seek innovative ways to contribute to the preservation and creation of affordable housing in our communities. To that end, UPMC Health Plan is seeking partners to spur investment in essential affordable housing. We invite partners to join us in working to preserve existing affordable housing options and supporting supplemental new construction in opportunity neighborhoods. Together, we can prevent displacement and create vibrant communities.
Learn more:
- Containing health care costs by getting homeless people into housing and out of the ER, WESA, May 2018
- Medicaid expansion may boost homeless individuals' access to care, HealthPayer Intelligence, Jan. 2021
- Healthy investments: Leveraging health plan capital for affordable housing and community development, Community Catalyst
Get in touch
When thinking about how to address the social needs of the community, it can often seem like the sky is the limit. In order to maximize our impact, we intend to grow intentionally into new areas. We are focused on testing social interventions and their impact on the health, quality, and cost of our members and the community. Email us directly at socialimpact@upmc.edu to explore opportunities to collaborate with us.
References
1. Magnan S. Social determinants of health 101 for health care: Five plus five. NAM Perspectives. Discussion Paper. October 9, 2017. National Academy of Medicine, Washington, DC.
2. World Health Organization (WHO). Social determinants of health. WHO. Accessed February 1, 2021. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
3. Joint Center for Housing Studies of Harvard University. Housing America’s older adults: Meeting the needs of an aging population. 2014. Joint Center for Housing Studies of Harvard University. Cambridge, MA.
4. Enterprise Community Partners, Inc. Renters report housing costs significantly impact their health care. Enterprise Community Partners, Inc. April 3, 2019. Accessed February 1, 2021. https://www.enterprisecommunity.org/news-and-events/news-releases/2019-04_renters-report-housing-costs-significantly-impact-their-health-care
5. Cunningham M, MacDonald G. Housing as a platform for improving education outcomes among low-Income children. May 2012. Urban Institute. Washington, DC.
6. Brennan M, Reed P, Sturtevant LA. The impacts of affordable housing on education: a research summary. November 2014. Center for Housing Policy, a division of the National Housing Conference. Washington, DC.
